Pathophysiology and Clinical Manifestations of Diarrhea
Diarrhea is an increase in the frequency of bowel movements, an increase in the looseness of stool or both.
Diarrhea is caused by increased secretion of fluid into the intestine, reduced absorption of fluid from the intestine or rapid passage of stool through the intestine.
Pathophysiology of Diarrhea
The basic mechanisms that cause diarrhea are the first osmotic disruption, due to the presence of food or substances that are not absorbed will cause the osmotic pressure within the gut cavity rises, resulting in a shift of water and electrolytes into the intestinal cavity, excessive intestinal cavity contents, will stimulate the intestines to remove, causing diarrhea.
Second, due to certain stimuli (such as toxins) in the gut wall will be an increase of water and electrolytes into the gut cavity and subsequent diarrhea arises because there is an increase in intestinal cavity contents.
Third, motalitas intestinal disorders, the hyperperistaltic, will lead to less opportunity to absorb food intestine causing diarrhea, conversely, when the peristaltic intestinal bacteria decreases will result in excessive arise later can also cause diarrhea.
Besides diarrhea may also occur, due to the entry of microorganisms living in the gut after successfully passing through the stomach acid barrier, microorganisms proliferate, then release toxins and toxin occurs due to hypersecretion which in turn will cause diarrhea.
While the result of the diarrhea will occur of the following:
1. Loss of water (dehydration)
Dehydration occurs due to water loss (output) more than income (input), is the cause of death in diarrhea. Disorders of acid-base balance (metabik acidosis)
It occurs due to loss of Na-bicarbonate with feces. Lipid metabolism is not perfect so dirty stuff accumulate in the body, the accumulation of lactic acid due to anorexia tissue. Acidic metabolic products are increasing due to be issued by the kidneys (oliguria occurs / anuria) and the removal of Na ions from the extracellular fluid into the intracellular fluid.
2. Hypoglycemia
Hypoglycemia occurs in 2-3% of children suffering from diarrhea, more often in children who had previously been suffering from protein-calorie deficiency. This occurs because of the interference of storage / supply of glycogen in the liver and disruption of glucose absorption. Symptoms of hypoglycemia will occur if the blood glucose levels were 40 mg% in infants and 50% in children.
3. The occurrence of weight loss in a short time, this is caused by:
Food is often stopped by parents, for fear of diarrhea or vomiting intensified.
Although milk passed, often given to expenditures and of diluted milk was given too long.
Food given often can not be digested and absorbed properly because of hyperperistaltic.
4. Impaired circulation
As a result of diarrhea, hypovolemic shock can occur, resulting in reduced tissue perfusion and hypoxia, acidosis gain weight, can cause brain bleeding, decreased consciousness, and if not addressed client will die.
Clinical Manifestations of Diarrhea
- At first, children / baby whiny anxiety, body temperature may be increased, decreased appetite.
- Frequent bowel movements with liquid or watery stool consistency.
- Stool color changed to greenish due to mixed bile.
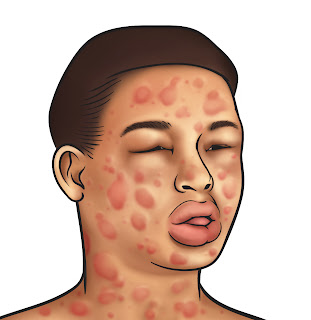
- Anus, and surrounding blisters because of frequent bowel movement and stool becomes more acidic due to the amount of lactic acid.
- There are signs and symptoms of dehydration, clear skin turgor, fontanel and sunken eyes, dry mucous membranes and with weight loss.
- Changes in vital signs, pulse and respiration rapid drop in blood press, rapid heart rate, the patient is very weak, decreased consciousness (apathy, samnolen, sopora komatus).
- Reduced diuresis (oliguria to anuria).
- If metabolic acidosis occurs, the client will look pale and breathing fast and deep.